Could Loss of Smell from COVID-19 Create Future ‘Dementia Wave’?
Olfactory bulb damage may have lasting effect on cognitive function in ‘smell long haulers’
By the American Physiological Society (Original release here.)
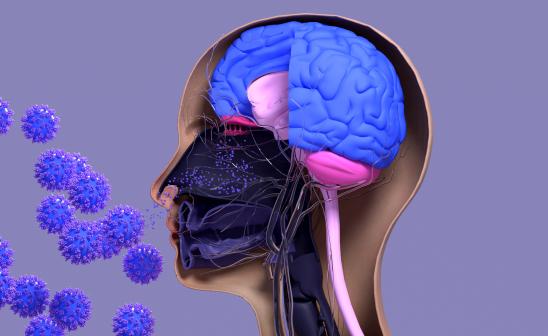
A review of studies about the effect of SARS-CoV-2—the virus that causes COVID-19—on the olfactory system introduces questions about whether loss of smell associated with COVID-19 infection may increase the risk of developing dementia later in life. The review, by Leslie Kay, professor in the Department of Psychology at The University of Chicago, is published ahead of print in the Journal of Neurophysiology (JNP).
Loss of smell (anosmia) is one of the hallmark symptoms associated with the first wave of COVID-19 in 2020, with an estimated 77–85% of people infected with the virus reporting loss or alteration of smell (parosmia). Although most people recover quickly from this dysfunction, an estimated 15 million people around the world are considered “smell long haulers” after otherwise recovering from COVID-19. They experience persistent anosmia or parosmia.
Studies have shown that the olfactory sensory epithelium—located in the upper area of the nose, close to where the olfactory nerve enters the olfactory bulb in the brain—carries a high viral load in people infected with SARS-CoV-2. The olfactory bulb is the structure in the brain that manages the sense of smell and sends sensory information to other areas of the brain for processing. These other brain regions are involved with learning, memory and emotion.
“All of this means that the [olfactory bulb] is involved in much more than smelling. It’s involved in the sense of place, memory, context, emotion, reward and many other processes,” said Kay.
Due to the proximity of the olfactory sensory epithelium to the olfactory bulb, COVID-19 infection could affect cognitive function even after recovery. A correlation between disrupted sense of smell and dementia has also been found in some people with neurodegenerative conditions such as Alzheimer’s and Parkinson’s disease. Animal studies have shown that damage to the bulb results in anxiety and a depression-like state.
Previous pandemics also lend support to the theory that “viral invasion of the [central nervous system] can be a trigger for neurodegeneration resulting in later neurological deficit,” Kay explained. The 1918 Spanish influenza pandemic led to a wave of people who developed Parkinson’s disease, and data from Denmark find that people who have had the flu have a 70% higher risk of developing Parkinson’s disease a decade later.
The review offers evidence that suggests inflammation introduced to the olfactory nerve and damage to the olfactory bulb via COVID-19 infection and immune response may also cause degeneration of brain structures connected to the olfactory system and cognitive impairment.
More research is needed and is possible due to the technological advances available to scientists during the current pandemic, Kay said. “While a catastrophe on many levels, the COVID-19 pandemic presents an opportunity to improve human health.”
Read the full article, “COVID-19 and olfactory dysfunction: a looming wave of dementia?,” published ahead of print in the Journal of Neurophysiology (JNP).
 THE UNIVERSITY OF CHICAGO
THE UNIVERSITY OF CHICAGO

